Better Claims Processing Means Better Healthcare
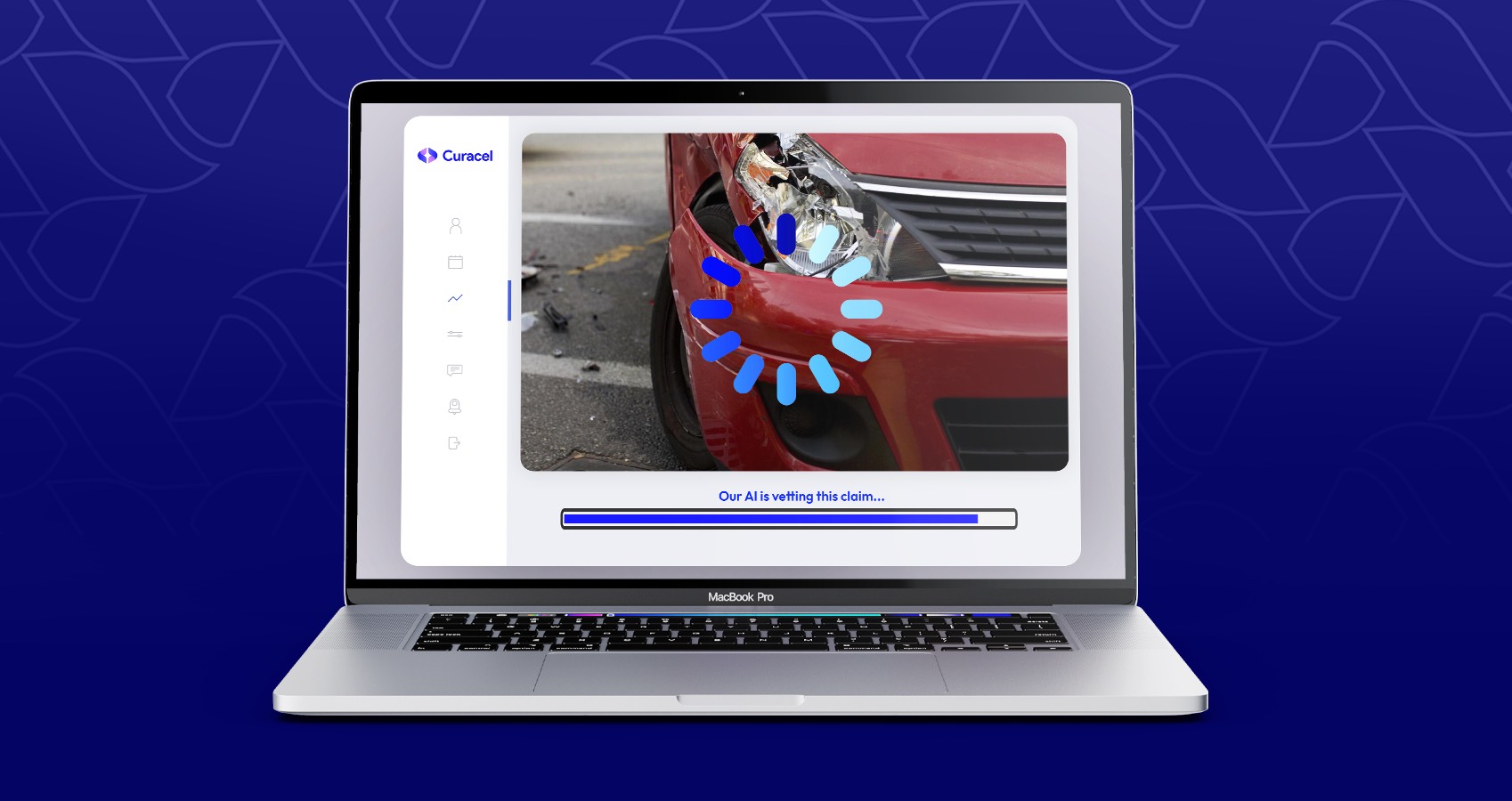
Technology has the potential to significantly reduce the cost of claims processing.
For healthcare providers, claims processing can be a cumbersome process. It requires having a knowledge of tech and using the right tech tool, as well as attention to detail to ensure that the claims are processed correctly and promptly. To make this process as efficient as possible, it's important to adopt a digital-first approach.
Digital-first for healthcare claims processing means to think about all aspects of the business — starting at the point of service through final settlement — in a digital context.
Sounds easy, but the harder task is figuring out how to get there - and what.
For Healthcare Providers. You should be able to choose.
You have a choice to make when it comes to how you handle claims transactions online. You can use an online claim submission system, or you can use your existing systems. If you're already processing claims, the decision is easy — go ahead and complete the transactions online. 😎
Consider making the switch
But if you need to make a switch, you may wonder how much of your information will be transferred along with your data. Both options are similar in that they both involve submitting claims through a Web form. The difference is that one involves uploading data, while the other involves sending it electronically via email.
The biggest advantage of using an online claim submission system like Curacel is that you don't have to send any of your data by email. This is especially true if there are sensitive health information involved, like medical diagnoses. But there are also risks connected with sending electronic data via email — some servers may be more susceptible to attacks than others, for example. This is one of the places where health insurance fraud happens.
If you choose to send health claims in an electronic format, then steps should be taken to verify that everything has been received correctly. And since this process takes time, it's important to plan for it not to delay your processing schedule unduly.
The insurance bills.
Health insurers and healthcare providers and other healthcare agencies are in a tricky position when it comes to billing disputes. They can't afford to make mistakes on the front end, because those errors can cost them thousands of dollars in lost revenue. Read this.
Healthcare providers, also can't afford to pay for medical costs out of pocket for a bill that's later proven to be erroneous. So, any way you slice it, healthcare providers are in a tough spot when it comes to billing consistency because their livelihoods depend on it. And the growth of the business.
For the patient with a health insurance policy
If you have health insurance, chances are your provider has a claims processing department. But it pays to know what kinds of claims they handle and the process they use.
Claims processing departments typically handle two types of claims:
First, they process pre-existing medical conditions that may arise during a covered period. These include things like cancer, heart disease or pregnancy. They also handle things like pneumonia during a hospital stay, which isn't considered pre-existing but still needs to be reported to the insurer. Pre-existing conditions don't need to be reported to the insurer if there's no indication of them when you enroll in the plan; if you enroll after being diagnosed with cancer, for example, it needs to be reported as such.
The second type is new medical conditions that develop during a covered period. These are defined by what happens:
• Lost workday absence resulting from an accident or physical illness that happened while you were insured
• Injury or illness that occurred while you were insured and is treated by a health care provider
• Injury or illness that occurred while you were insured and is treated by a health care provider and is not related to abortion or miscarriage
• Pregnancy loss resulting from an accident or physical illness
Claims Processing Done Right
Technology offers immense potential for enhancing the efficiency of claims processing - in time and money spent, as well as accuracy and security. The ability to process large volume, high-velocity transactions quickly, accurately, and at lower cost cannot be achieved without technology-enabled solutions.
It is important to document, process and analyze all claims to ensure compliance. If you are experiencing problems in your claims management, Curacel Claims Automation can help.
We can help you streamline your compliance processes and ensure your claims are processed accurately and on time.
After all, why file paper forms when you can file your claims electronically? 😊
Subsribe to our newsletter to receive weekly content























.svg)



